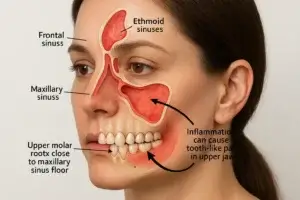
A stuffy nose, facial pressure, and thick mucus can make any day miserable. But not every sinus infection needs antibiotics. In fact, most are viral and clear on their own, while a smaller number are bacterial and benefit from targeted treatment. There is also a third, often overlooked cause in adults, sinus infections that originate from a dental problem. Knowing the difference helps you feel better faster and prevents unnecessary antibiotics or repeated flare ups.
Quick refresher, what counts as a sinus infection?
Sinus infections happen when the lining of your sinuses becomes inflamed and swollen, trapping mucus and causing pressure and pain. Acute rhinosinusitis is usually triggered by a common cold. Most cases are viral and improve within 7 to 10 days. Only a small proportion convert to bacterial sinusitis.
- The American Academy of Family Physicians notes that about 0.5 to 2 percent of viral colds become acute bacterial sinusitis in adults. You can review their guidance in the AAFP overview of acute rhinosinusitis.
- The Infectious Diseases Society of America outlines specific signs that point to bacterial disease, especially the duration and pattern of symptoms.
Relevant sources: IDSA clinical practice guideline for acute bacterial rhinosinusitis, AAFP current concepts in adult acute rhinosinusitis, and CDC information on sinus infections and antibiotic use.
Viral vs bacterial vs dental origin, the key differences
When you pay attention to timing, severity, and laterality, you can often tell what is most likely going on.
| Feature | Viral Sinusitis | Bacterial Sinusitis | Dental Origin Sinusitis |
|---|---|---|---|
| Typical timeline | Peaks around day 3–5, starts improving by day 7 | Symptoms persist 10+ days, severe early symptoms for 3–4 days, or worsen again after initial improvement | Often lingers or recurs until the dental issue is treated |
| Fever | None or low-grade | High fever (39°C / 102.2°F), may occur early | Usually none |
| Nasal discharge | Clear to colored, improves by a week | Persistent purulent discharge or returns after early improvement | Often one-sided, foul odor or bad taste |
| Facial pain/pressure | Diffuse pressure, worse when bending over | Moderate to severe, localized, may be one-sided | One-sided cheek pain, pain in upper molars, pain when chewing or tapping a specific tooth |
| Other clues | Improves with rest and supportive care | Does not improve or worsens, affects daily function | Recent dental work, deep cavity, failing root canal, or gum infection |



